
- MEDICARE TIMELY FILING CODE
- MEDICARE TIMELY FILING PLUS
- MEDICARE TIMELY FILING PROFESSIONAL
MEDICARE TIMELY FILING CODE
The five character codes included in the Aetna Precertification Code Search Tool are obtained from Current Procedural Terminology (CPT ®), copyright 2022 by the American Medical Association (AMA). Click on "Claims," "CPT/HCPCS Coding Tool," "Clinical Policy Code Search." Visit the secure website, available through for more information. MEDICARE TIMELY FILING PROFESSIONAL
Aetna defines a service as "never effective" when it is not recognized according to professional standards of safety and effectiveness in the United States for diagnosis, care or treatment. All services deemed "never effective" are excluded from coverage.Not all plans are offered in all service areas.
MEDICARE TIMELY FILING PLUS
Applies to: Aetna Choice ® POS, Aetna Choice POS II, Aetna Medicare ℠ Plan (PPO), Aetna Medicare Plan (HMO), all Aetna HealthFund ® products, Aetna Health Network Only ℠, Aetna Health Network Option ℠, Aetna Open Access ® Elect Choice ®, Aetna Open Access HMO, Aetna Open Access Managed Choice ®, Open Access Aetna Select ℠, Elect Choice, HMO, Managed Choice POS, Open Choice ®, Quality Point-of-Service ® (QPOS ®), and Aetna Select ℠ benefits plans and all products that may include the Aexcel ®, Choose and Save ℠, Aetna Performance Network or Savings Plus networks. It does not mean precertification as defined by Texas law, as a reliable representation of payment of care or services to fully insured HMO and PPO members. The term precertification here means the utilization review process to determine whether the requested service, procedure, prescription drug or medical device meets the company's clinical criteria for coverage. Should the following terms and conditions be acceptable to you, please indicate your agreement and acceptance by selecting the button below labeled "I Accept". In the event that a member disagrees with a coverage determination, member may be eligible for the right to an internal appeal and/or an independent external appeal in accordance with applicable federal or state law. Medical necessity determinations in connection with coverage decisions are made on a case-by-case basis. Please note also that the ABA Medical Necessity Guide may be updated and are, therefore, subject to change. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. 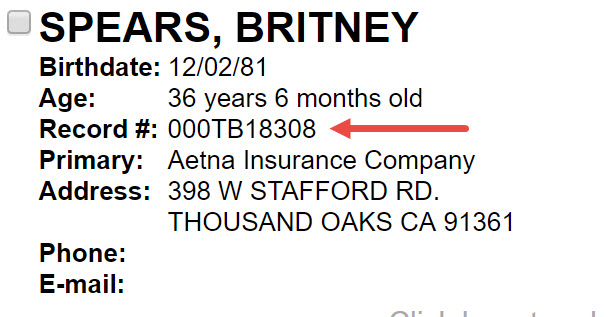
The member's benefit plan determines coverage. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna) for a particular member.
Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. Members should discuss any matters related to their coverage or condition with their treating provider.Įach benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Treating providers are solely responsible for medical advice and treatment of members. The ABA Medical Necessity Guide does not constitute medical advice. The Applied Behavior Analysis (ABA) Medical Necessity Guide helps determine appropriate (medically necessary) levels and types of care for patients in need of evaluation and treatment for behavioral health conditions. Our Compliance Department completes random audits to ensure compliance on an annual basis.īy clicking on “I Accept”, I acknowledge and accept that: You can access the training and attestation at the link(s) below. Providers continue to be notified via OfficeLink Newsletters during the summer months.
Delegated Entities: Provider attestation collection for the FDR compliance requirements continue to be required for Delegated Entities.Īnnual notification regarding requirements will be sent to providers via Adobe Acrobat Sign email or postcard. MA/ D-SNP/FIDE: Providers who are in states/regions that offer MA/D-SNP/FIDE plans are required to complete an Annual D-SNP Model of Care (MOC) training and attestation. MA/MMP: Providers who participate only in our MA/MMP plans do not need to complete an annual FDR Attestation. 
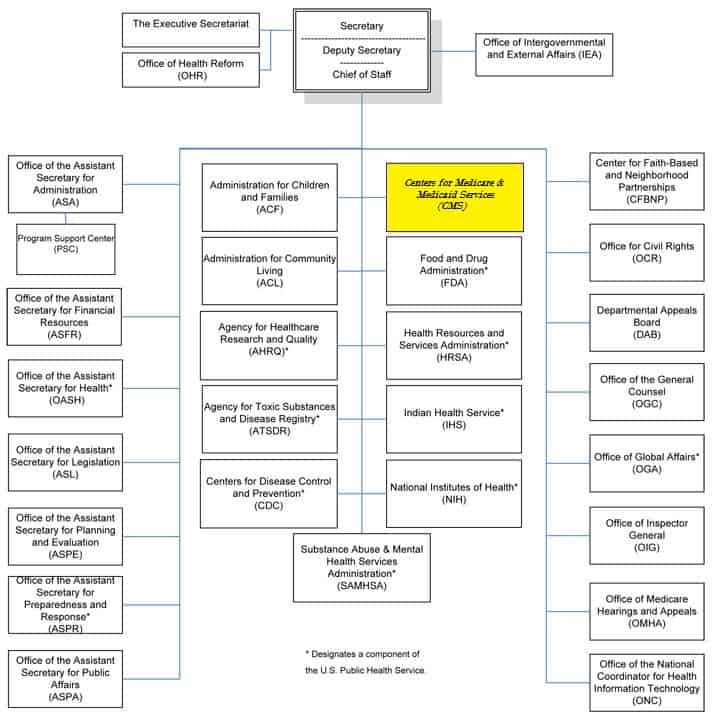
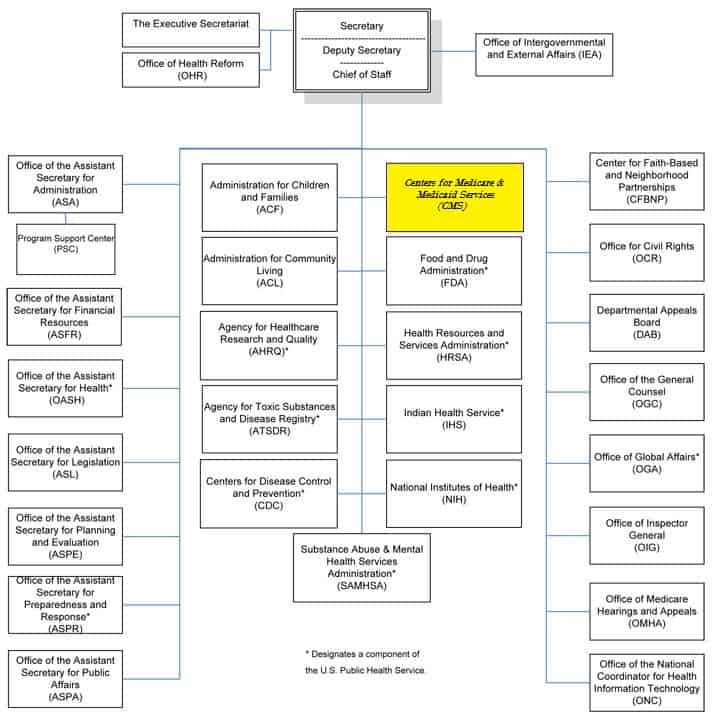
New and existing participating providers in our Medicare Advantage (MA), Medicare-Medicaid (MMP), Dual Eligible (D-SNP) or Fully Integrated (FIDE) Special Needs Plans are required to meet the Centers for Medicare & Medicaid Services (CMS) compliance program requirements for first-tier, downstream and related entities (FDR) as identified in the Medicare compliance FDR program guide and/or D-SNP Model of Care (MOC) training. Important: Annual Medicare Compliance Program Requirements





 0 kommentar(er)
0 kommentar(er)
